INTRODUCTION
Sometimes people get a thought running through their Head that just wont go away , like when a song gets struck in one’s mind. If that particular thought causes a lot of anxiety , it can become the basis for an OBSESSIVE-COMPULSIVE DISORDER , or OCD .
DEFINITION
OCD is a disorder ( what is disorder first of all , The term “disorder” generally refers to a condition characterized by a disturbance in normal functioning, structure, or behavior of a person, organism, or system. In various fields, such as medicine (physical or mental health), psychology, and biology, the term is often used to describe a deviation from the normal or expected state ) in which intruding thoughts that occur again and again ( obsessions , such as fear that germs are on one’s hands) are followed by some repetitive , ritualistic behavior or mental acts ( compulsions , such as repeated hand washing , counting, etc ) . The complusions are meant to lower the anxiety caused by the thought. IT FALLS UNDER MAJOR PSYCHOLOGICAL DISODER.
MAJOR CHARACTERSTICS
In literature’s most famous case of obsessive compulsive disorder , Lady Macbeth cries , “Out , damn’d spot! out , I say ! ” as she repeatedly washes her hands , trying to rid herself of guilt foe the murder of King Duncan . Although people with OCD dont usually hallucinate about blood spots on their hands , Shakespeare get the rest spot-on . The main characteristics of OCD are PERSISTENT , Unwelcome thoughts and ritual behaviors . Many parents check their baby’s breathing often at first . Everyone has a little obsessive thoughts on occasions or some small ritual that makes them makes them feel better. The difference is whether a person likes LIKES to perform the ritual ( but doesn’t have to) or feels COMPELLED to perform the ritual and feels extreme anxiety if unable to do so . The distress caused by a failure or an inability to successfully complete the compulsion is defining feature of OCD .
OCD SYMPTOMS ( OBSESSIVE COMPULSIVE DISORDER )

Symptoms of OCD:
- Obsessions :
a)Intrusive and unwanted thoughts, images, or urges.
b)Fear of contamination or germs.
c)Disturbing thoughts about harming oneself or other d)Need for symmetry, perfection, or exactness.
2.Compulsions:
Repetitive behaviors or mental acts performed in response to obsessions.
Checking and rechecking things.
Washing or cleaning excessively.
Counting or repeating words silently.
TYPES OF OCD ( OBSEESIVE COMPULSIVE DISORDER )
OCD manifests in various forms, and individuals may experience a combination of different obsessions and compulsions. Common subtypes include:
1.Contamination OCD: Fear of germs or contamination.
2.Checking OCD: Constantly checking things, such as locks or appliances.
3.Symmetry and Ordering OCD: Needing things to be in a particular order or symmetry.
4.Hoarding OCD: Difficulty discarding possessions, leading to clutter.
TREATMENT FOR OCD ( OBSEESIVE COMPULSIVE DISORDER )
- DRUG THERAPIES
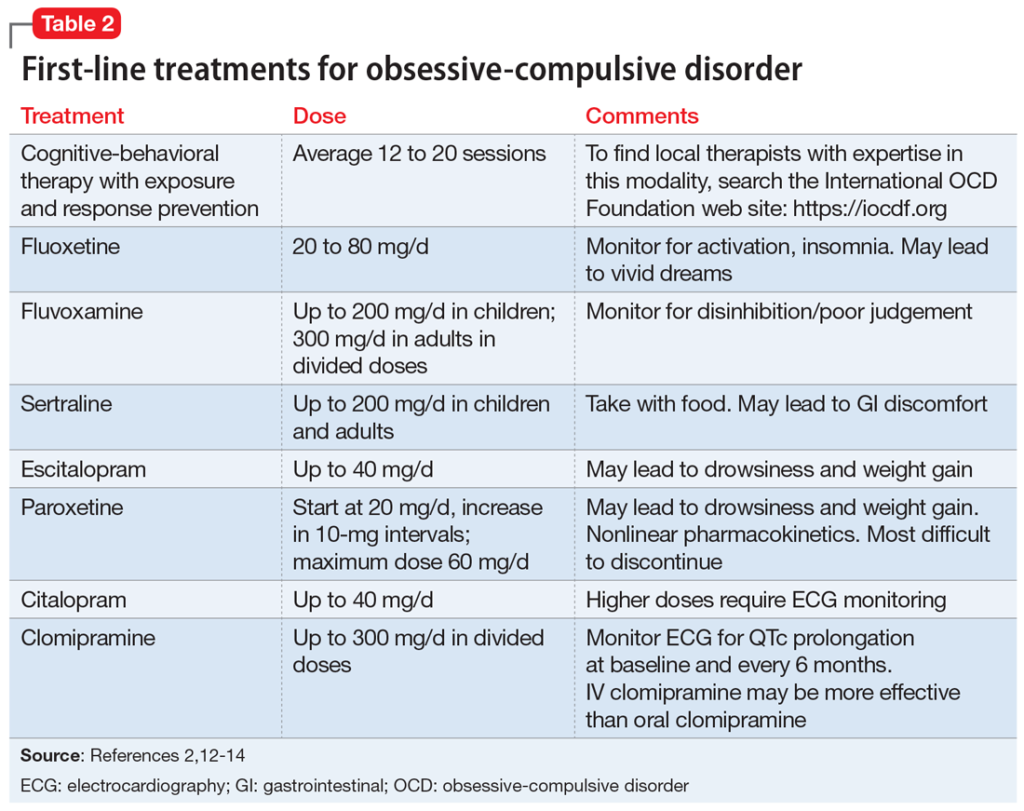
2. BEHAVIORAL THERAPY
Cognitive-Behavioral Therapy (CBT):
Exposure and Response Prevention (ERP) is a specific type of CBT effective for OCD.
Involves gradually facing feared obsessions and resisting the accompanying compulsions.
3. Deep Brain Stimulation (DBS)
In severe cases, where other treatments haven’t been effective, DBS may be considered.
Is There a Cure for OCD? While there isn’t a cure for OCD, many individuals find significant relief through treatment. With the right combination of therapy and medication, individuals can manage symptoms effectively and lead fulfilling lives. Early intervention is crucial for better outcomes.
NEUROSCIENCE BEHIND OCD ( OBSESSIVE COMPULSIVE DISORDER)
Obsessive-Compulsive Disorder (OCD) has been studied extensively from a neuroscience perspective, and researchers have identified several key brain areas and neurotransmitters involved in the disorder. While our understanding is continually evolving, here are some insights into the neuroscience behind OCD:
Brain Structures:
Basal Ganglia: The basal ganglia, a group of structures deep within the brain, is thought to play a crucial role in the development of OCD. Specifically, abnormalities in the circuit connecting the orbitofrontal cortex, thalamus, and basal ganglia are implicated.
Orbitofrontal Cortex (OFC): The OFC is responsible for decision-making and reward processing. Dysfunction in this area is associated with the inability to suppress intrusive thoughts or impulses.
Cingulate Cortex: The anterior cingulate cortex, a part of the brain’s limbic system, is involved in error detection and emotional processing. Changes in this area may contribute to the anxiety and distress experienced by individuals with OCD.
Neurotransmitters:
Serotonin: Imbalances in serotonin, a neurotransmitter that regulates mood and anxiety, are often implicated in OCD. Selective serotonin reuptake inhibitors (SSRIs), a class of antidepressant medications, are commonly used to treat OCD and work by increasing serotonin levels in the brain.
Dopamine: Dysregulation of dopamine, another neurotransmitter, has also been linked to OCD. Changes in dopamine levels may influence the reward system and contribute to compulsive behaviors.
Neurocircuitry and Functional Connectivity:
Functional neuroimaging studies, such as fMRI (functional Magnetic Resonance Imaging) and PET (Positron Emission Tomography), have provided insights into the abnormal connectivity between different brain regions in individuals with OCD. Altered communication within the orbitofrontal-striatal-thalamic circuitry is a common finding.
Genetics:
There is evidence suggesting a genetic component in the development of OCD. Certain genes associated with serotonin regulation and the glutamate system have been implicated.
Environmental Factors:
Traumatic events or significant life stressors may contribute to the onset or exacerbation of OCD symptoms. The interaction between genetic predisposition and environmental factors is an area of ongoing research.
Understanding the neuroscience of OCD has led to the development of effective treatments, including medication and cognitive-behavioral therapy (CBT). Research in this field continues to explore the intricate interplay between genetics, brain structures, and neurotransmitter systems to refine our understanding of OCD and improve therapeutic interventions.
CONCLUSION
Obsessive-Compulsive Disorder (OCD) is a complex mental health condition that involves a combination of genetic, neurobiological, and environmental factors. The neuroscience behind OCD highlights the involvement of specific brain structures, neurotransmitters, and functional connectivity abnormalities. While there is no definitive cure, various effective treatments, including cognitive-behavioral therapy and medication, can help individuals manage and alleviate symptoms.
Understanding the interplay between the brain, genetics, and environmental factors is crucial for tailoring treatment approaches. Ongoing research in neuroscience continues to shed light on the intricate mechanisms of OCD, offering hope for more targeted interventions in the future. It’s important to approach OCD with empathy, recognizing the challenges individuals face and the impact it can have on their daily lives.
SOME FAQS ON OCD ;
What is Obsessive-Compulsive Disorder (OCD)?
OCD is a mental health condition characterized by persistent, unwanted thoughts (obsessions) and repetitive behaviors or mental acts (compulsions) performed to alleviate anxiety.
What causes OCD?
The exact cause of OCD is not fully understood, but a combination of genetic, neurobiological, and environmental factors is believed to contribute to its development.
How is OCD diagnosed?
Mental health professionals diagnose OCD based on a thorough assessment of symptoms using criteria outlined in the Diagnostic and Statistical Manual of Mental Disorders (DSM-5).
What are the common treatments for OCD?
Treatment options include cognitive-behavioral therapy (particularly Exposure and Response Prevention), medication (such as SSRIs), and in some cases, deep brain stimulation.
Is there a cure for OCD?
While there is no definitive cure, many individuals find significant relief through a combination of therapy and medication. Early intervention and ongoing management are essential for symptom control.
Can OCD be prevented?
There is no guaranteed way to prevent OCD, but early recognition of symptoms and prompt intervention can help manage the condition effectively.
How does OCD affect daily life?
OCD can significantly impact daily functioning, leading to distress and disruption in relationships, work, and overall quality of life. Seeking professional help is crucial for improved coping and management.
Is OCD common?
OCD is a relatively common mental health disorder, affecting people of all ages and backgrounds. It is estimated that about 2% of the global population experiences OCD at some point in their lives.
Remember, if you or someone you know is struggling with OCD, seeking guidance from a mental health professional is essential for proper diagnosis and tailored treatment.

